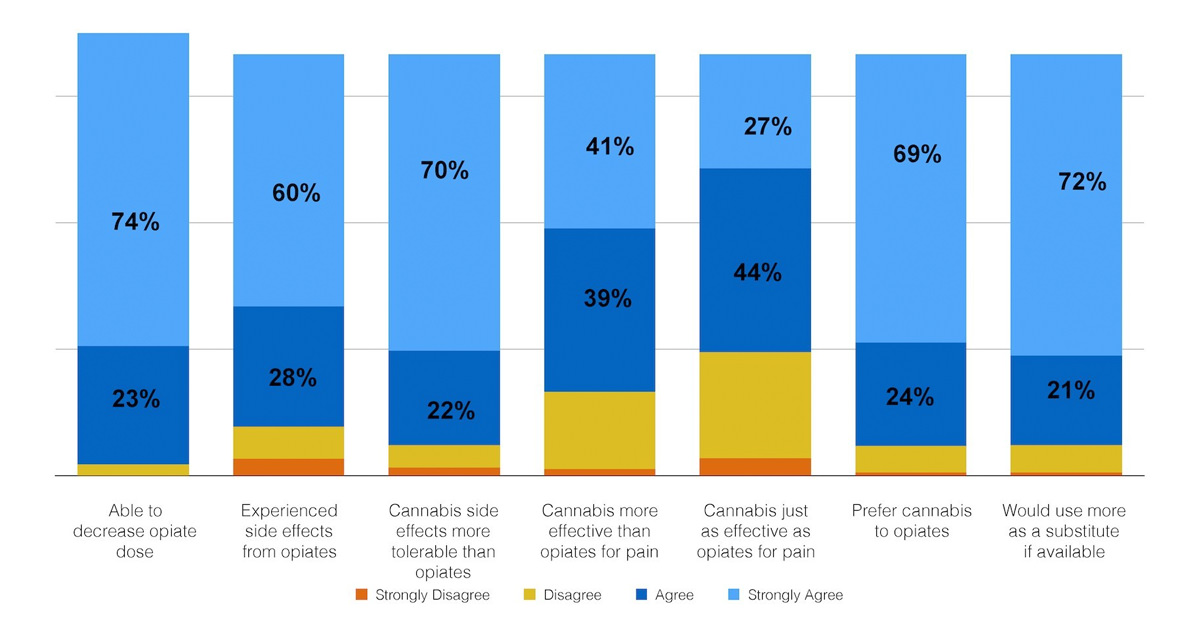
Pain patients would rather use cannabis than opiates, a new study found. In a survey of nearly 3,000 medical marijuana patients, 97 percent of respondents said they could decrease their opioid use with the help of cannabis. Just over 80 percent said that cannabis alone was more effective than taking opioids in conjunction with cannabis, and 92 percent said they preferred cannabis to treat their condition. About 600 of the participants said they use cannabis and opiates together.
Conducted by UC Berkeley and Hello MD, a medical marijuana website through which the researchers found all 3,000 participants, the survey offered further proof that cannabis can substitute opiate painkillers.
This research comes at a key time, in the midst of conversations on the federal level about America’s opioid crisis. Overdose fatalities are on the rise in the United States, with more than 60 percent of them involving opioids. According to the CDC, every day 91 Americans die from an opioid overdose, including both prescription pills and heroin.
“I feel like we’ve hit a wall,” says Amanda Reiman, co-leader of the study and vice president of community relations for Flow Kana, a cannabis distribution company in San Francisco. Marijuana’s status as a Schedule I controlled substances prohibits researchers from conducting large-scale clinical trials to further investigate cannabis as a replacement for opiates.
Nonetheless, in practice individual patients, harm reduction organizations, and the High Sobriety rehab facility in Los Angeles, have already begun to make or support that substitution.
“What I really wanted to do with this study was collect enough data that other researchers could use as a jumping off point for getting into those more clinically minded assessments {to determine} whether this is a viable treatment or protocol,” Reiman tells Jane Street. With a robust database, she wanted to look at more nuanced factors, like gender and ethnic differences, when it comes to using opioids and substituting them with cannabis.
“Pain is overwhelmingly the condition for which people are using cannabis,” says Reiman, citing conditions like back pain, migraines, PMS, and fibromyalgia. She also found that women are more likely than men are to report using opioids in the past six months. “When we look at gender differences, is there a higher risk of opioid issues among women?” Reiman asks. Women are also more likely to ingest cannabis via non-inhalation methods, she added. “When trying to think about how we attract women into using medical cannabis, when they may be at higher risk of opioid dependence and overdose, we should look at non-inhalation methods.”
Moreover, the survey asked respondents if they’d be more likely to use cannabis if it were more available and less stigmatized. Reiman found that people of color overwhelmingly responded yes to this question. “We see the intersectionality of marginalization and stigmatization that is heightened for this population,” she says. Especially when African Americans are nearly four times as likely to be arrested for weed, they may be more reticent to fully embrace a Schedule I drug as medicine — even if it’s a healthier alternative to painkillers.
Reiman also found that older people were more likely to have taken opioids in the past six months than younger people. Populations to look out for regarding opioid dependence and overdose are women and older adults, she says. “They’re also the fastest growing adopters for medical marijuana,” Reiman adds. “This is an opportunity for education directed at these populations in medical marijuana states. The products available to them impact the rates of overdose in this population specifically.” In support of Reiman’s point, states with medical marijuana have seen a 25 percent decrease in opioid overdose deaths as compared to their prohibitionist counterparts.





